I woke up one Tuesday morning and couldn’t grip my coffee mug properly. My fingers felt stiff, almost swollen, and my knees ached as I walked down the stairs. At 54, I’d been navigating menopause for two years, but this joint pain felt like a whole new level of discomfort. Sound familiar? You’re definitely not alone. Research shows that more than 70% of us experience joint pain during menopause, and honestly, nobody warned me it would be this intense. Here’s what I’ve learned after countless conversations with my doctor and trying various supplements for menopause and joint pain: this isn’t just about aging. It’s about hormones, inflammation, and finding what actually helps your body thrive through this transition.
Why Does Menopause Cause Joint Pain in the First Place?
Here’s what’s really happening. When our hormones shift during menopause, it’s like our body’s natural cushioning system starts breaking down. That estrogen we’re losing? It was quietly protecting our joints all along, and now we’re definitely feeling the difference.
What I’ve noticed is that the pain isn’t the same for everyone. Some women feel it mostly in their hands and fingers, while others struggle with knee or hip pain. For me, it was my hands in the morning and my knees after sitting too long. I recall the first time I couldn’t twist open a new jar of almond butter at my favorite coffee shop in Pasadena. At 54, I felt embarrassed asking the barista for help with something I’d always done easily. That’s when I knew I needed to take this seriously.
The hormonal changes can lead to stiffness, swelling, and that frustrating feeling of losing strength in your joints. But here’s the encouraging part: the right supplements for menopause and joint pain can genuinely make a difference.
The Top 5 Supplements That Actually Help
Omega-3 Fatty Acids: The Inflammation Fighter
Omega-3s were the first supplement my doctor recommended, and now they sit right next to my coffee maker so I never forget my morning dose. These essential fatty acids work by calming inflammation throughout your body, including in your joints. Studies show that women taking omega-3 supplements daily experienced significant reductions in joint pain and stiffness within about 12 weeks.
I started with a quality fish oil supplement (look for ones with the active ingredients clearly listed on the label), and within about six weeks, I noticed my morning stiffness wasn’t as severe. You can also get omega-3s from fatty fish like salmon or from algae-based supplements if you’re a vegetarian. Living in California, I’m lucky to have access to great fresh fish at our farmers’ markets, which makes it easier to get omega-3s from food, too.
Vitamin D: More Than Just Bone Health
Most of us think of vitamin D for bone health, which is crucial after 50. But it also plays a role in reducing joint pain. Lower vitamin D levels have been linked to increased joint discomfort in postmenopausal women.
What surprised me was learning that many women our age are deficient in vitamin D, especially if we’re diligent about sunscreen (which we should be). Even here in sunny Southern California, I was below optimal levels when I got tested. After supplementing for about three months, not only did my joint pain improve, but I felt more energetic during my morning walks along the beach. For personalized guidance on optimal vitamin D intake during menopause, it’s worth diving deeper into dosage recommendations
Collagen Peptides: Rebuilding What’s Been Lost
Collagen is what gives our cartilage structure and cushioning. During menopause, our bodies produce less of it, which contributes to that creaky, achy feeling in our joints. Research suggests that supplements containing collagen can help protect cartilage, improve joint function, and reduce joint pain.
I add collagen powder to my morning smoothie now. It’s flavorless, dissolves easily, and within a couple of months, I noticed my knees felt more stable when I climbed stairs. Not every collagen supplement is created equal, though, look for easily absorbed collagen powder or peptides specifically.
Glucosamine and Chondroitin: The Classic Combination
You’ve probably heard of this duo. They’re natural compounds found in cartilage, and some studies have found that glucosamine can help protect cartilage and reduce pain in people with osteoarthritis in their knees.
I’ll be honest: the research is mixed on these supplements, and they took longer to show benefits for me (about three months). But my book club friends and I compare notes on what’s working, and several of them swear by this combination. They’re worth discussing with your doctor, especially if you’re dealing with osteoarthritis alongside menopause symptoms.
Curcumin (Turmeric): Nature’s Anti-Inflammatory
Turmeric has been used for centuries in traditional medicine, and modern research backs up its benefits. Curcumin has powerful natural compounds that help keep cells healthy and decrease inflammation, which can reduce pain and improve movement in joints and muscles.
I keep turmeric capsules on hand and take them with black pepper (which helps your body absorb them better). The anti-inflammatory effects are real, though they’re more subtle than something like ibuprofen. Think of curcumin as part of your overall inflammation-fighting strategy rather than a quick fix.

What About Magnesium and Calcium?
While these minerals are essential for bone health after 50, their direct impact on joint pain is less clear. Magnesium helps with muscle relaxation and may ease tension around joints, while calcium supports bone density. I take both as part of my overall wellness routine, but I don’t rely on them specifically for joint pain relief.
If you’re curious about how calcium and vitamin D work together, especially during menopause, there’s valuable information about optimizing these nutrients after 50
Making Supplements Work Better: My Practical Tips
Here’s what I wish someone had told me from the start: supplements aren’t magic pills. They work best as part of a bigger picture.
Movement matters. I know it seems counterintuitive when your joints hurt, but gentle movement actually helps. I started with water aerobics at my local community pool and yoga classes designed for women over 50. Both were easier on my joints than my usual weekend hikes in the Santa Monica Mountains. The combination of omega-3 supplements and regular movement made a bigger difference than either one alone.
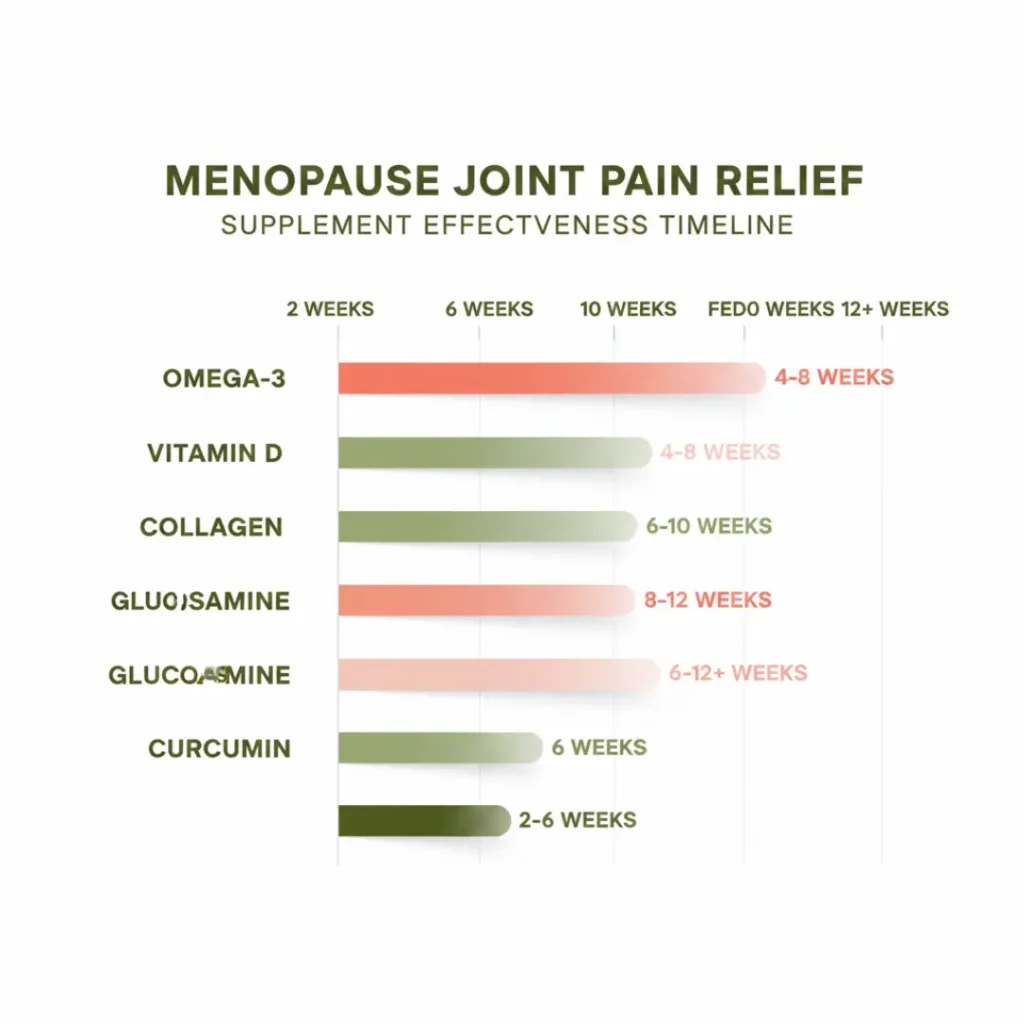
Give it time. Most supplements for menopause and joint pain need at least 6-8 weeks to show real benefits. Don’t give up after two weeks. I mark my calendar to reassess after two months.
Quality counts. Not all supplements are created equal. Look for third-party testing labels on the bottle to ensure you’re getting what the label promises.
Food first, when possible. I try to get nutrients from food whenever I can fatty fish for omega-3s, leafy greens for vitamin K, bone broth for natural collagen. Living in California means year-round access to fresh produce at farmers’ markets, which makes eating anti-inflammatory foods so much easier. Supplements fill the gaps.
What About Hormone Replacement Therapy?
This is worth mentioning because many women find that hormone replacement therapy (HRT) helps with joint pain by addressing the root cause: declining estrogen. I’m not on HRT, but several friends are, and they’ve noticed significant improvement in their joint pain.
If your joint pain is severe or affecting your quality of life, talk with your doctor about whether HRT might be appropriate for you. It’s not right for everyone, but it’s an option worth discussing alongside supplements. For a comprehensive overview of managing all menopause symptoms, including joint pain, consider exploring different treatment approaches.
When Should You See a Doctor?
Please don’t ignore severe or worsening joint pain. While menopause-related joint discomfort is common, you want to rule out other conditions like rheumatoid arthritis or osteoarthritis.
See your doctor if you experience sudden, severe joint pain, significant swelling or redness, pain that interferes with daily activities, or symptoms in one specific joint that’s getting progressively worse. These could signal something beyond typical menopausal changes.
Frequently Asked Questions
Your Journey Forward
Joint pain during menopause doesn’t have to sideline you from the active, vibrant life you deserve. While supplements for menopause and joint pain aren’t overnight solutions, they can provide genuine relief when used consistently and thoughtfully.
Remember, your body is going through a significant transition, and it deserves patience and support. Start with one or two supplements that resonate most with your symptoms, give them adequate time to work, and always keep your doctor in the loop. I’ve found that combining the right supplements with gentle movement, good nutrition, and self-compassion makes the biggest difference. You’re not just managing symptoms you’re supporting your body to thrive through this next chapter.



