Here’s something nobody tells you about menopause: the finish line isn’t where you think it is. Most of us assume the worst part is when our periods finally stop. We brace ourselves for that moment, thinking once we cross it, we’ll find relief on the other side. But what if I told you that the real challenge hits long before that day arrives? Understanding what the hardest stage of menopause is isn’t just helpful information—it’s the difference between feeling blindsided and feeling prepared when your body decides to turn everything upside down.
The answer: late perimenopause takes the crown
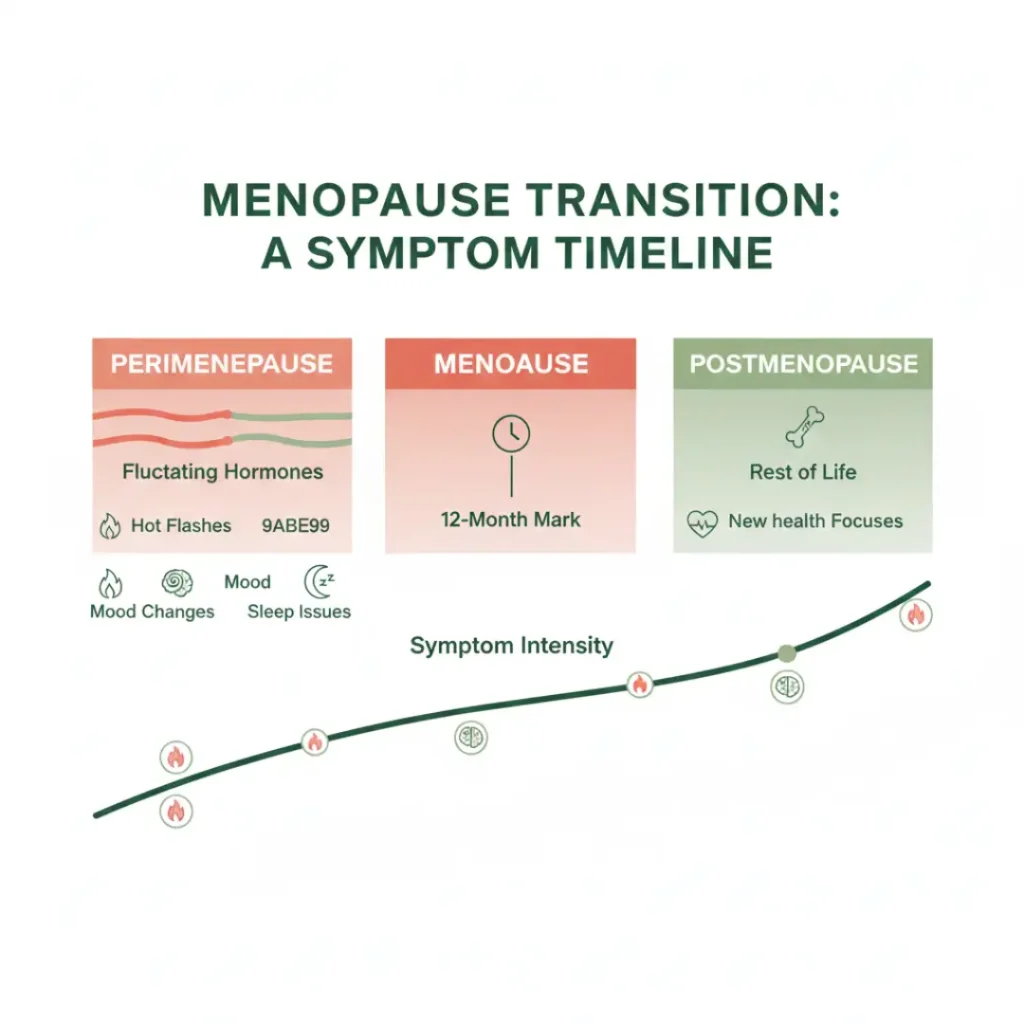
If you’ve been wondering what the hardest stage of menopause is, here’s the truth that surprises most women: it’s late perimenopause, which is the 1-3 years right before your final period, and it’s when your body’s hormonal roller coaster reaches its wildest peaks and valleys.
Why does this phase hit so hard? During late perimenopause, your estrogen levels don’t just decline gradually; they swing dramatically from day to day, sometimes hour to hour. One moment, you might have nearly normal estrogen levels, and the next, they’ve plummeted. Your body struggles to adapt to this unpredictability, and that’s what creates those intense symptoms everyone talks about.
Research shows that up to 80% of women experience severe hot flashes and night sweats during this phase. Many women dealing with menopause fatigue describe this period as the most exhausting of the entire transition. Sleep becomes elusive, mood swings feel overwhelming, and brain fog makes simple tasks frustrating.
What makes late perimenopause particularly brutal is how multiple symptoms pile on simultaneously. Poor sleep due to night sweats exacerbates mood changes, and hormonal chaos affects concentration. The sheer unpredictability leaves you feeling like you’re losing control of your own body. But here’s what I want you to know: you have more power than you think to ease this transition through simple, everyday lifestyle choices.
What does your daily routine need during the hardest stage
Let me share what I’ve learned works during this challenging phase. It’s not about complete life overhauls, it’s about smart, strategic adjustments to your daily routine that make a real difference.
Start your morning intentionally. Instead of reaching for your phone the moment you wake up, try this: open your curtains first. Exposure to natural light within 30 minutes of waking helps regulate your circadian rhythm, which is already disrupted by hormonal changes. Even five minutes of morning sunlight on your face signals your body to produce cortisol at the right time, setting you up for better sleep that night.
Your breakfast matters more than ever now. I’m talking about building a plate that stabilizes blood sugar and supports hormone balance. Think Greek yogurt (plain, not sweetened) topped with a handful of walnuts and fresh berries, or try two scrambled eggs with avocado on whole-grain toast and a side of sautéed spinach. The Mediterranean diet breakfast approach works beautifully here.
Healthy fats, quality protein, and fiber keep energy steady and hot flashes less frequent.
Add these vital vitamins women 50 need at breakfast through real food first. That yogurt? Is it giving you calcium and vitamin D? Those walnuts? Omega-3s for brain health and mood stability, spinach, and Magnesium help with sleep and reduce anxiety.
Move your body, but smartly; you don’t need intense workouts that stress your already stressed system. What works during late perimenopause is consistent, moderate movement. A 30-minute walk after breakfast does wonders; it improves insulin sensitivity (important for weight management), boosts mood through endorphins, and helps regulate body temperature.
I’ve found that strength training twice a week makes a noticeable difference. You don’t need a gym membership, simple bodyweight exercises at home, squats while you wait for your coffee to brew, wall push-ups while dinner cooks, and holding a plank during commercial breaks. These movements preserve muscle mass that naturally declines during this phase and support bone health.
Managing hot flashes through lifestyle: what actually works
Let’s talk about hot flashes during menopause and the lifestyle strategies that truly help. Medical treatments exist and work well, but these practical adjustments can reduce frequency and intensity significantly.
Your wardrobe becomes a tool. I keep three layers ready every morning: a breathable cotton camisole, a button-front cardigan (easier to remove quickly than pullovers), and a lightweight scarf or jacket. Natural fabrics, cotton, linen, and bamboo, allow your skin to breathe. Avoid polyester and other synthetics that trap heat and moisture.
Keep a “hot flash kit” in your bag: a small battery-powered fan, cooling wipes, and a water bottle. I learned this from a friend who swore it saved her during business meetings. When a flash hits, having these tools within reach makes it manageable instead of mortifying.
Temperature control at home and work. Set your bedroom thermostat between 60-67°F at night. Yes, it seems cold, but it’s optimal for sleep during this phase. Invest in moisture-wicking sheets (bamboo or special athletic fabric) and keep a cooling pillow on hand. Layer blankets so you can adjust easily when night sweats hit.
At work, position yourself near windows you can open or away from heat sources. Keep a small desk fan handy. If you work from home, this is easier to control; embrace it.
Trigger awareness changes everything. Start tracking what sets off your hot flashes. Common culprits include spicy foods, hot beverages, alcohol (especially red wine), caffeine after 2 PM, and stress. You don’t have to eliminate everything forever, but knowing your triggers helps you make conscious choices. Maybe you skip the spicy curry on days when you have important meetings scheduled.
Sleep strategies that actually work during late perimenopause
Understanding why sleep problems increase after age 50 helps you tackle them strategically. Hormonal fluctuations directly impact sleep architecture, but your evening routine can work with your body instead of against it.
Create a cooling bedtime ritual. About an hour before bed, take a lukewarm shower, not hot, which slightly lowers your core body temperature, signaling sleep time. Follow with a lightweight, breathable nightgown or pajamas, and keep a second set on your nightstand for when night sweats require a change.
Your bedroom should become a sleep sanctuary. Remove electronic devices; the blue light disrupts melatonin production, which is already compromised by hormonal changes. Use blackout curtains or an eye mask. Consider a white noise machine to mask disruptive sounds that wake you during lighter sleep phases.
The 3-2-1 rule works wonders: No food 3 hours before bed (prevents acid reflux that worsens with hormonal changes), no liquids 2 hours before bed (reduces nighttime bathroom trips), no screens 1 hour before bed (protects melatonin production). Replace evening scrolling with reading, gentle stretching, or journaling.
If night sweats wake you, don’t just lie there frustrated. Get up, change your clothes if needed, do some gentle stretches, sip cool water, then return to bed. Fighting wakefulness creates anxiety around sleep, making the problem worse.
Nutrition and supplements: your daily defense
What you eat directly impacts how you feel during the hardest stage of menopause. Let me be specific about what helps.
Build every meal around these principles: Include protein (aim for 25-30 grams per meal to maintain muscle mass and stabilize blood sugar), add healthy fats (avocado, olive oil, nuts, fatty fish), and fill half your plate with vegetables. This combination keeps you satisfied longer and reduces those energy crashes that make everything feel harder.
Certain foods deserve special mention. Flaxseeds contain lignans that may help with hot flashes. Grind them fresh and add a tablespoon to your morning smoothie or yogurt. Soy foods (edamame, tofu, tempeh) contain phytoestrogens that some women find helpful. Cold-water fatty fish (salmon, sardines, mackerel) provide omega-3s that support mood and reduce inflammation.
What to minimize: Refined sugars and simple carbs cause blood sugar spikes and crashes that worsen mood swings and energy fluctuations. Alcohol, especially in the evening, disrupts sleep quality even if it helps you fall asleep initially. Excessive caffeine intensifies anxiety and triggers hot flashes in many women.
Consider these supplements for perimenopause and beyond after discussing with your doctor: Vitamin D3 (2000-4000 IU daily) with K2 for bone health, magnesium glycinate (300-400mg before bed) for sleep and muscle relaxation, omega-3 fatty acids (1000-2000mg daily) for mood and heart health, and a quality B-complex for energy support.
Stress management: your secret weapon
Stress amplifies every menopause symptom. When you’re stressed, cortisol levels spike, which interferes with already-disrupted hormone balance. The good news? Simple stress management practices make a measurable difference.
Practice 4-7-8 breathing when hot flashes strike: Breathe in through your nose for 4 counts, hold for 7 counts, exhale through your mouth for 8 counts. This activates your parasympathetic nervous system, helping regulate body temperature and reducing anxiety. Do this three times whenever you feel a hot flash coming or when stress peaks.
Gentle yoga, especially restorative poses, helps tremendously. You don’t need an hour-long class. Even 10 minutes of cat-cow stretches, child’s pose, and legs-up-the-wall pose before bed calms your nervous system. There are wonderful free videos online specifically for menopause symptoms.
Social connection matters more than you think. Isolation makes symptoms feel worse. Schedule regular coffee dates, join a walking group, or find online communities of women going through the same thing. Talking about your experience with others who understand reduces the psychological burden significantly.
Set boundaries without guilt. If evening social events exhaust you during this phase, it’s okay to decline. If you need to leave work on time instead of staying late, do it. Protecting your energy isn’t selfish; it’s essential self-care during a demanding transition.
When lifestyle adjustments need medical support
Everything I’ve shared helps, but I want to be clear: lifestyle changes don’t always solve everything, and that’s completely normal. If your symptoms remain severe despite these adjustments, medical treatment isn’t a failure; it’s smart healthcare.
Hormone replacement therapy can be life-changing for women struggling with severe symptoms during late perimenopause. Non-hormonal options exist, too. Some women benefit from antidepressants that reduce hot flash frequency. Others find relief with blood pressure medications that weren’t designed for menopause but happen to help with temperature regulation.
Don’t suffer in silence because you think you “should” be able to manage this naturally. Late perimenopause is intense for biological reasons beyond your control. Combining lifestyle strategies with appropriate medical treatment when needed gives you the best quality of life during this transition.
Talk with a healthcare provider who listens and takes your concerns seriously. If your doctor dismisses your symptoms as “just menopause” without offering solutions, find a new doctor. You deserve support, not dismissal.

Looking toward postmenopause: life gets better
Here’s the hopeful truth about what is the hardest stage of menopause: it’s temporary. Once you cross into postmenopause, that 12-month mark without a period, most women experience significant relief as hormones stabilize at new, lower levels.
Hot flashes typically decrease in frequency and intensity within 2-5 years after your final period. Sleep improves. Energy returns. That brain fog lifts. Many women describe feeling more like themselves again, often with deeper self-knowledge and confidence than before.
The lifestyle habits you build during late perimenopause serve you beautifully in postmenopause and beyond. That morning walk becomes a cherished routine. The Mediterranean-style eating supports heart and brain health long-term. The stress management practices enhance overall well-being for years to come.
Understanding perimenopause vs menopause and postmenopause helps you recognize that you’re moving toward a phase many women describe as liberating. No more periods. No pregnancy concerns. Often, renewed clarity about what truly matters in life.
If you’re looking for more ways to thrive with energy, confidence, and vitality at 50, remember that this transition, though challenging, can become a gateway to one of your most vibrant decades.
Your next steps
So what is the hardest stage of menopause? For most women, it’s late perimenopause—those intense 1-3 years before periods stop. But you now have specific, practical strategies to ease the journey.
Start with one or two changes rather than trying to overhaul everything overnight. Maybe this week, you can focus on your morning routine and sleep environment. Next week, you will adjust your breakfast and add a daily walk. Small, consistent changes compound into significant relief over time.
Track what helps. Keep a simple journal noting symptoms, lifestyle adjustments, and how you feel. This helps you identify patterns and gives you concrete information to share with your healthcare provider.
Remember, you’re not alone in this journey. Millions of women navigate this transition every year. The support and information available today far surpass what previous generations had access to. Use it. Reach out. Connect with others. Advocate for yourself.
Always consult with a qualified healthcare provider about your specific symptoms and treatment options. Your experience is unique, and personalized medical advice ensures you get the support that’s right for your body and circumstances.
The hardest stage passes, and what comes next holds genuine possibility for vitality, purpose, and joy. What small lifestyle change will you try first this week?



