When my doctor revealed that my vitamin D levels were alarmingly low, it all started to make sense. I’d been battling exhaustion, body aches, and mood swings symptoms I had dismissed as just menopause. In reality, my body was desperately signaling its need for more vitamin D. If you’re asking, ‘How much vitamin D should a menopausal woman take?’ you’re addressing one of the most crucial health questions for this stage of life. While the answer isn’t universal, understanding your body’s specific needs can truly transform how you feel every single day.
Why Menopause Changes Your Vitamin D Needs
I had been struggling with exhaustion, body aches, and mood swings, symptoms I had brushed off as part of menopause. However, understanding how menopause affects the entire body can help manage these symptoms more effectively. Here’s something many women don’t realize; menopause doesn’t just mess with your periods and temperature regulation. The drop in estrogen fundamentally changes how your body handles vitamin D. When estrogen levels decline, we become less efficient at both producing vitamin D from sunlight and absorbing it from food. It’s like our bodies suddenly forgot the recipe they’d been following for decades.
But there’s more. Research published in recent studies shows that women with vitamin D levels below 20 ng/mL experienced more severe menopausal symptoms, lower bone density, and reduced quality of life compared to women with adequate levels above 30 ng/mL. This isn’t just about preventing osteoporosis down the road, it’s about feeling vibrant and strong right now.
Lower estrogen also means your gut absorbs less calcium, which is where vitamin D becomes your secret weapon. Lower estrogen also means your gut absorbs less calcium, which is where vitamin D becomes your secret weapon. For comprehensive guidance on balancing vitamin D and calcium for bone health, explore our complete calcium and vitamin D guide. Vitamin D helps your body grab onto that calcium and put it where it belongs: in your bones, not floating uselessly through your bloodstream. Think of vitamin D as the delivery truck that makes sure calcium actually arrives at its destination.
The Right Dosage: What the Science Actually Says
The standard recommendation you’ll find on most vitamin bottles 600 IU for women under 70; is honestly just a starting point. What I’ve learned through research and conversations with healthcare providers is that most postmenopausal women need considerably more to achieve optimal blood levels.
According to medical experts, if your baseline vitamin D levels are low (and many postmenopausal women do have low levels), you’ll typically need an extra 1,000 IU beyond your daily multivitamin to reach that sweet spot of 30-65 ng/mL. Studies examining vitamin D supplementation in menopausal women found that daily doses over 2,000 IU were necessary to raise deficient levels to at least 20 ng/mL within a year.
Here’s a practical breakdown:
- Baseline maintenance: 600-800 IU daily (what’s in most multivitamins). To understand if you need additional supplementation beyond a multivitamin, explore our complete guide to choosing a safe 50+ formula.
- Additional supplementation for deficiency: 1,000-2,000 IU extra
- Total daily intake: Often 1,000-2,800 IU for menopausal women
- Safe upper limit: 4,000 IU per day
One caveat: these are general guidelines. Your ideal dose depends on your current vitamin D levels, where you live, how much time you spend outdoors, your skin tone, and your overall health. This is why I always recommend getting your blood levels tested before starting supplementation, then retesting after three months to see where you land.
Vitamin D3 vs. D2: Why the Type Matters
Not all vitamin D supplements are created equal, and this genuinely matters for menopausal women. Vitamin D3 (cholecalciferol) is the form your skin naturally produces from sunlight, and it’s significantly better absorbed by your body than vitamin D2 (ergocalciferol). When you’re shopping for supplements, always look for D3 on the label.
Here’s a tip that made a real difference for me: vitamin D is fat-soluble, which means you’ll absorb it much more efficiently when you take it with food that contains some fat. I take mine with breakfast alongside my morning eggs or avocado toast. You don’t need a fatty meal just a little healthy fat helps your body make the most of your supplement.
Many experts also recommend pairing vitamin D3 with vitamin K2, especially for menopausal women concerned about bone health. These two vitamins work together in calcium metabolism, with K2 helping direct calcium into your bones rather than your arteries. It’s a partnership that supports both bone density and cardiovascular health.
Recognizing Vitamin D Deficiency During Menopause
The tricky thing about vitamin D deficiency is that its symptoms often masquerade as normal menopause complaints. For the longest time, I thought my constant tiredness was just part of the package. Turns out, my body was trying to tell me something specific.
Common symptoms of low vitamin D in menopausal women include:
- Persistent fatigue that sleep doesn’t fix
- Bone and muscle aches, especially in your back, hips, and legs can signal low vitamin D. If you’re experiencing persistent joint discomfort, learn about targeted supplements for menopause related joint pain.
- General weakness and feeling unwell
- More intense menopausal symptoms
- Low mood or increased anxiety
- Frequent infections or illnesses
- Poor bone density on screening tests
Severe deficiency can lead to osteomalacia, a condition where your bones literally soften. This is different from osteoporosis (where bones become brittle), but equally concerning. The good news? Correcting vitamin D deficiency often brings noticeable improvements in energy, mood, and physical comfort within weeks.
Beyond Bones: How Vitamin D Supports Your Whole Body
We tend to think of vitamin D purely as a bone health nutrient, but during menopause, it does so much more. Research shows vitamin D plays crucial roles in mood regulation, immune function, and even vaginal health. Women with adequate vitamin D levels often report better management of menopausal symptoms overall.
Vitamin D supports the production of serotonin, that feel-good neurotransmitter that helps regulate mood. This connection explains why vitamin D deficiency is linked to increased anxiety and depression during menopause. When you’re already navigating hormonal shifts, having adequate vitamin D gives your brain the tools it needs to maintain emotional balance.
Your immune system also relies heavily on vitamin D to function properly. During menopause, when inflammation can increase throughout your body, vitamin D acts as a natural anti-inflammatory agent. The study I mentioned earlier found that women with vitamin D deficiency showed heightened inflammation markers compared to those with adequate levels.
How to Optimize Your Vitamin D Strategy
Getting enough vitamin D during menopause requires a multi-pronged approach. Supplements are important, but they work best alongside other strategies. I like to think of it as building a vitamin D portfolio rather than relying on a single source.
Sensible sun exposure: About 10-15 minutes of midday sun on your arms and legs several times a week helps your skin produce vitamin D naturally. Obviously, balance this with skin cancer prevention we’re not talking about sunbathing for hours. And if you live in northern latitudes or it’s winter, sun exposure alone won’t cut it.
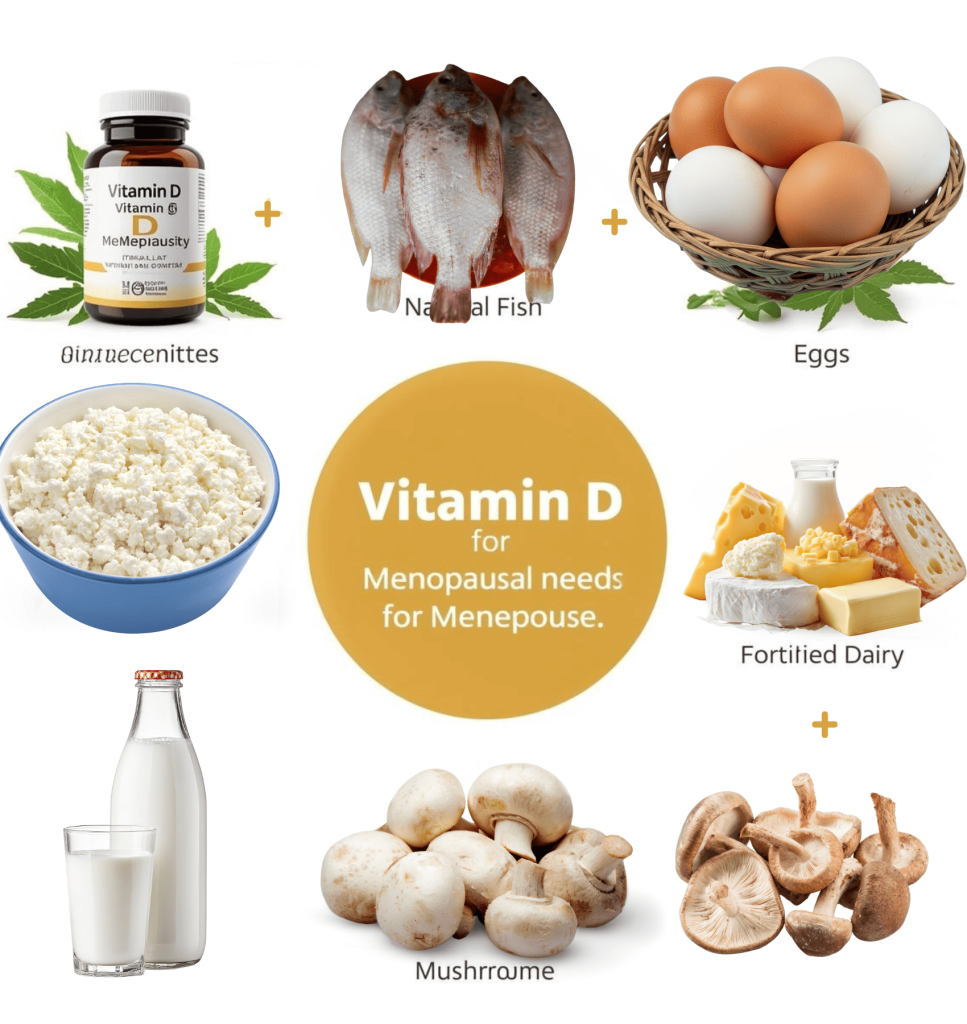
Vitamin D-rich foods: Fatty fish like salmon and mackerel, fortified dairy or plant milks, egg yolks, and mushrooms exposed to UV light all contribute to your intake. While it’s hard to get enough from food alone, every bit helps build your baseline.
Quality supplementation: Choose vitamin D3 supplements from reputable brands that undergo third-party testing. Look for doses in the 1,000-2,000 IU range for daily use, and consider combination formulas with K2 and magnesium for enhanced absorption.
Regular monitoring: Ask your doctor to check your 25 hydroxyvitamin D blood levels annually or whenever you adjust your supplementation. This simple blood test shows exactly where you stand and takes the guesswork out of dosing.
Special Considerations and When to Adjust Your Dose
Certain factors might mean you need more vitamin D than the average menopausal woman. If you have darker skin, you naturally produce less vitamin D from sun exposure and may need higher supplementation. The same goes if you live in northern states like Washington or Maine, where winter sunlight is too weak for vitamin D production for several months.
Women with conditions affecting fat absorption—like Crohn’s disease, celiac disease, or those who’ve had gastric bypass surgery often need higher doses because vitamin D absorption is compromised. If you’re taking certain medications, including some cholesterol-lowering drugs or steroids, these can interfere with vitamin D metabolism.
Being significantly overweight can also affect vitamin D status, as the vitamin gets sequestered in fat tissue and becomes less available to your body. This doesn’t mean supplementation doesn’t work it just means you might need slightly higher doses to achieve optimal blood levels.
Frequently Asked Questions
Taking the Next Step
Understanding how much vitamin D should a menopausal woman take empowers you to take control of this foundational aspect of your health. Whether you need 1,000 IU or 2,000 IU daily depends on your individual circumstances, but the evidence is clear: adequate vitamin D supports your bones, mood, immune system, and overall quality of life during this transition. Learn more about meeting your B12 needs through natural food sources by clicking here.
I encourage you to schedule a vitamin D blood test with your healthcare provider if you haven’t had one recently. Knowing your baseline takes the guesswork out of supplementation and helps you target the dose that’s right for your body. Remember, while these guidelines provide a solid foundation, your doctor can help tailor recommendations to your specific health profile, medications, and individual needs. You deserve to feel your absolute best during menopause and beyond. For comprehensive guidance on thriving through this transition, explore our honest, empowering menopause guide.



